Gail Gates- Med Five Results
Information obtained by phone interview 8/29 with Dr. Roberts and his review of Mr. Gates 6/05 CT angiogram and stress echo reports, and the 11/03 and 6/05 reports from Mr. Gates Cardiologist. The 11/03 angiographic report and stress echo reports, and prior lab work have been requested. Just because Gail seems to have improved on the Med Fivedoesn’t mean that others will.
What happens in Vegas shouldn’t stay in Vegas
That is, if you want your arteries to open up
Gail Gates is a 70 year old, moderately active, non-diabetic, non-smoking man with a 30 year history of hypertension, well controlled medically. His cholesterol has been elevated, above 250 mg/dl, and he has not wished to take cholesterol lowering drugs.
In the late fall of ’03, Gail felt poorly – “out of gas” – activities previously well tolerated left him short of breath and fatigued. A stress echo study returned abnormal, leading to invasive coronary angiography, which revealed a culprit 80% narrowing within the Left Anterior Descending (LAD) coronary artery, which serves the front wall of Gail’s heart. This narrowing was successfully balloon dilated and stented. A second artery contained a significant but non-critical 60% narrowing and Gail’s third coronary artery, a non-threatening 40% constriction. A non-severe, asymptomatic calcific narrowing of Gail’s aortic valve was noted.
A repeat stress echo study was carried out post-stent placement. Gail walked for 6 minutes; his heart rate did not rise to target, as he was on Atenolol (a Beta-blocking drug, which lowers your HR and BP) but no abnormalities were identified, indicating that the stented artery was open and that the other two narrowings were not a current threat. Atenolol was continued for a period of time; Plavix, an anticoagulant platelet inhibitor, was continued for 6 months (standard practice after stent placement). Mr. Gates cholesterol was around 250 mg/dl. Lipitor therapy was advised; Mr. Gates was concerned about side-effects and took this agent only briefly. Thus his cholesterol remained elevated.
In the late winter/early spring of this year (’05) Mr. Gates began to experience a recurrence of his original symptoms. Activity that was previously well tolerated now left him fatigued and short of breath. Symptom severity was not as bad as in 11/03, but something was definitely wrong. Mr. Gates is a resident of Iowa City, Iowa, but he was in Las Vegas, working on a temporary assignment, when his cardiac symptoms returned. He learned of the Med Fivefrom Janet Kelly’s radio program, and began Rejuvetate on 3/20/05. Gail felt better. Three months later his energy level and effort tolerance were back to normal. Gail also noticed an improvement in GI function and in his overall sense of well being.
Gail had returned to Iowa City from Las Vegas and was scheduled to see his Cardiologist in 4/05; she was out of town and the exam was rescheduled for mid 6/05. At this point Gail has been on Rejuvetate for three months.
Gail’s 6/16/05 stress echo returned normal; he walked for 6:00, now achieving a heart rate of 145 (he was no longer on Atenolol, the Beta-blocking drug). No evidence of coronary insufficiency was found. The mean pressure gradient across Gail’s aortic valve was 28 mmHg (reference is made to an echo obtained one year earlier that showed a similar, 25 mmHg gradient – this difference is well within the measurement variance range). Gail’s cardiologist gave him a clean bill of health.
Gail requested a CT angiogram; he wanted to see if the Med Fivehad had any affect on his underlying arterial disease. His cardiologist was skeptical but agreed to the study. When the results returned she called Gail personally, beginning the conversation with – “you’re going to like this”. The CT angiogram demonstrated that the stent site was patent (as expected, given the current absence of symptoms and the negative stress study). Calcium was noted within the aortic valve, also expected, but what was not expected, and what is remarkable here, was the presence of only mild calcification within Gail’s coronary arteries, and
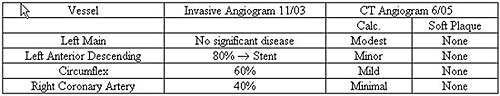
During an invasive coronary angiogram, such as Gail’s 11/03 study, we inject X-ray contrast dye directly into the coronary arteries; an X-ray movie of the dye filling the arteries is then obtained. The percentage of a given artery’s diameter that is narrowed by atherosclerotic plaque is described as it’s “percent stenosis”. This is not a direct measurement, but an eye-ball estimate. Different observers may vary by 10-20% in their estimate of a given artery’s percent stenosis, but we all typically agree on whether a narrowing is mild, moderate, or severe in degree. The CT angiogram, Gail’s 6/05 study, takes advantage of recent advances in computerized X-ray imaging. The same X-ray dye is used, but it is injected into an arm vein. Multiple X-ray slices are obtained through the heart and reconstructed by the computer to obtain crisp images of the coronary arteries. This is a new technology; there is only one such scanner in Iowa, and fortunately for Gail this scanner is in Iowa City. Now, as different imaging techniques were used (direct angiography in ’03 and CT angiography in ’05), in a sense an “apples to apples” comparison is not possible, but nonetheless, the degree of change is marked, and likely not due to technical differences between the exams or measurement error.
Artery wall calcification, in general, parallels the degree of soft plaque deposition and the percent stenosis of a given vessel. Artery wall calcification progresses at a rate of 20-40% per year. Unless active measures are taken, soft plaque deposition and vessel percent stenosis will progress as well. But on the 6/05 study, only modest calcification was seen in Gail’s arteries. No soft plaque was identified; the 60% and 40% narrowings observed in 11/03, in the two vessels that were not stented, just weren’t there anymore. This suggests that soft plaque had been resorbed, that the arteries had opened up. This is consistent with the resolution of Gail’s symptoms. This all occurred following only three months of Rejuvetate. I have never heard of anything like this. Aggressive lipid lowering therapy, aggressive phosphatidylcholine therapy, and aggressive chelation therapy may all have favorable affects on the degree of arterial blockage in one’s vessels, and I have seen this, but the affects are typically modest and take months to years to develop.
We would expect that Gail’s narrowings might have worsened between ’03 and ’05. While the symptoms he experienced in early ’05 could, in theory, have been due to a problem other that recurrent coronary disease, the odds are that a coronary blockage was the culprit. Thus the negative findings on Gail’s 6/05 CT angiogram are all the more remarkable, and suggest a rapid disease reversal.
Clara Forestieri’s carotid ultrasound findings improved when Rejuvetate was added to prior, long-standing, stain lipid lowering therapy. Following the addition of Rejuvetate, Clara’s HDL rose by 17%, from 52 to 61, and her ultrasound improved. I do not have in my possession Gail’s prior lipid panel results, but I know that his cholesterol had been elevated for some time, and that in 6/05 his cholesterol remained elevated at 245 mg/dl, with an LDL of 169 mmHg. If Rejuvetate opened up Gail’s coronary arteries, as appears to be the case, it did so by means other than via improved lipid control. We understand that high cholesterol is just one of the many factors that play a role in plaque formation. Statin lipid lowering drugs thus cannot be the “be all and end all” of coronary disease management; no drug can. Rejuvetate was designed to take aim at the causes of plaque deposition that are not currently being addressed by standard, drug based medicine. Rejuvetate alone will not be the “be all and end all” of coronary disease management, but Rejuvetate sure worked for Mr. Gates. Gail will remain on the Rejuvetate system. His CT angiogram can be repeated in the future; over time we might just see a reduction in aortic valve calcification as well. And remember –
What happens in Vegas shouldn’t stay in Vegas
That is, if you want your arteries to open up
James C. Roberts MD FACC 8/30/05
Do not use this product if you are pregnant or nursing. If you are under a physician's care or taking medication, consult your health professional before taking this product. If you are taking or intend to take other detoxification treatments while on MedFive, please discuss this with your physician first. You should take minerals and vitamins when using this product – supplements and medications should be taken at least two hours apart from Step Two. This product is not intended to diagnose, treat, cure, or prevent any disease.
It is not necessary to take other detox programs while on Med Five.
|
|